 |
Because the clinical and radiologic manifestations of fungal infection are often nonspecific, definitive diagnosis of fungal infections requires employing procedures with some degree of invasiveness. Tissue specimens for confirming a diagnosis of hepatosplenic candidiasis, for example, may be obtained via ultrasound-guided, fine-needle biopsy or laparoscopically.
Tissue specimens for the diagnosis of invasive pulmonary aspergillosis can be obtained by bronchoscopy. However, bronchoalveolar lavage (BAL) is frequently falsely negative, and biopsy cannot be performed in most patients with thrombocytopenia. In patients suspected of having aspergillosis, percutaneous fine-needle biopsy can also be used, although the yield is variable and dependent on location of the lesion. Peripherally located lesions are more accessible by percutaneous fine-needle biopsy. If open-lung biopsy, by either thoracoscopy or thoracotomy, can be safely performed, it provides the best tissue specimens.
Biopsy is particularly important in suspected fungal infection of the sinuses. Biopsy can not only provide evidence of mucosal invasion, but can also lead to the differentiation of aspergillosis from infections caused by other invasive fungi, eg, the Zygomycetes, which may require different treatment.
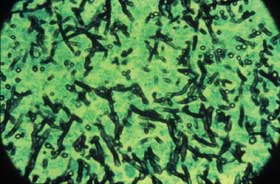
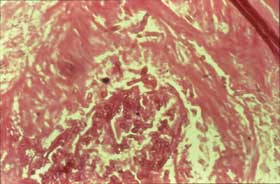
The presence of dichotomous-branching, septate, nonpigmented hyphae on direct microscopy usually indicates Aspergillus (Fig 8a). Gomori methenamine silver stain should be done to detect the hyphae, which are generally found in tissue with extensive necrosis, hemorrhagic infarcts, and vascular invasion. However, Aspergillus hyphae are almost impossible to distinguish from those of Scedosporium, Pseudallescheria, and Fusarium spp, which are emerging as important pathogens in the HSCT population. The hyphae of the Zygomycetes are irregular, broad, and non-septate (Fig 8b). Nonetheless, only culture can definitively distinguish among the various hyphae-bearing fungi that may cause infection in the HSCT patient.

 |
|
Figure 8a: Lung tissue showing dichotomously branching septate hyphae, characteristic of invasive Aspergillus: methenamine silver stain.
|
Figure 8b: Pulmonary artery filled with broad, irregular non-septate hyphae indicative of invasive zygomycosis (Hematoxylin and Eosin stain).
|
Course Number: V035D
This CME Expires on July 1, 2005; no tests will be accepted after this date.
This course is accredited by
The University of Pittsburgh School of Medicine, Center for Continuing Education and The International Immunocompromised Host Society
|
 |

