 |
Radiologic examination – plain films, CT scans, MRIs, and ultrasound studies – can offer valuable clues to the presence of fungal infections in HSCT patients. These studies are especially useful when interpreted in concert with clinical findings, histologic and microbiologic data, and the state of immune recovery.34
Invasive Aspergillosis
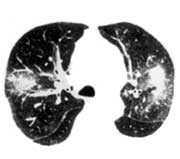
The negative and positive predictive values for chest radiographs are low in immunocompromised patients.35 Chest radiographs have been found to be normal in up to 25% of patients at the onset of invasive aspergillosis.35 Lesions of invasive aspergillosis can be patchy, peripheral, bilateral infiltrates, or solitary or multiple nodules. These lesions may progress over a period of days to weeks to form dense consolidated infiltrates, or cavitated nodules. Wedge-shaped, pleural-based lesions reminiscent of a segmental pulmonary infarction are characteristic (Fig 6a).
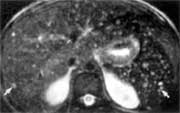
High-resolution CT scanning permits earlier and better assessment of the presence, pattern, and distribution of pulmonary abnormalities in invasive aspergillosis. Infiltrates and small nodules not appreciable on chest radiographs are shown, and pleural and pulmonary involvement can be differentiated. Two characteristic radiologic findings of aspergillosis are the halo sign and the air-crescent sign. The halo sign is an early manifestation, occurring even while patients are still neutropenic, and as such can be very useful in making an early diagnosis. The halo sign appears on high-resolution CT as a rim of ground-glass attenuation surrounding a nodule and corresponds, histologically, to a rim of hemorrhage surrounding a focus of pulmonary infarction (Fig 6b). The halo sign has been noted to precede air-crescent formation by 1 to 3 weeks.36 Air crescents usually do not appear until neutropenia resolves. The air-crescent sign corresponds to cavitation that occurs at the time of neutrophil recovery (Fig 6c).35 The diagnostic usefulness of this sign is therefore limited by the relatively late occurrence.

 |
 |

|
Figure 6a: Frontal x-ray of BMT patient with invasive pulmonary aspergillosis showing multiple bilateral nodules (arrowheads) and a peripheral wedge-shaped consolidation (arrow).
Reprinted with permission, Leung, et al. Radiology 1999;210:669-710.
|
Figure 6b: High-resolution CT scan shows 2 nodules, each with a surrounding halo of ground-glass attenuation.
Reprinted with permission, Worthy, et al. Radiographics 1997;17:1359-71.
|
Figure 6b:
Air crescents caused by angioinvasive aspergillosis as seen on high-resolution CT.
Reprinted with permission, Nucci personal communication.
|
While both the halo and air-crescent signs are highly suggestive, neither is specific for aspergillosis. Both have also been reported in a variety of pulmonary infections caused by other angioinvasive fungi, such as the Zygomycetes and Pseudallescheria boydii.37 Similar CT findings have been observed in patients with metastatic cancer38 and infection with mycobacteria and CMV.38,39
Thoracic MRI is not as helpful as CT scanning for the early diagnosis of IFI. The diagnostic value of MRI lies primarily in follow-up of later stages of the disease. The typical MRI finding in invasive aspergillosis is a nodular lesion with a lower signal in the center and an area of higher-signal intensity at the rim; these target-like lesions are visible on both T1- and T2-weighted images.
MRI is the radiologic tool of choice for detecting cerebral aspergillosis.40,41 MRI–detectable lesions are often multiple, frequently found in the basal ganglia, and resemble those associated with acute brain infarcts. It is noteworthy that over 90% of brain abscesses in the HSCT patient are caused by fungi.41-43
When Aspergillus or other angioinvasive fungi invade the sinuses, CT evaluation can detect disease earlier than standard sinus radiographs. CT is particularly helpful in detecting bony erosion. MRI is also a valuable diagnostic modality in these patients, especially for detecting fungal extension into the frontal lobe or the carotid artery in the area of the siphon.44
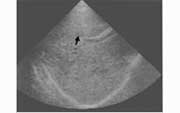
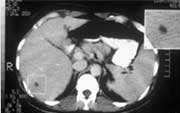
Hepatosplenic Candidiasis
MRI and CT are more sensitive than ultrasound in diagnosing hepatosplenic candidiasis (Fig 7). Lesions may not be detected by radiologic evaluation in neutropenic patients because they are unable to mount the necessary inflammatory response. Both MRI and CT will detect characteristic lesions in about 90% of patients, compared with 70% to 75% with ultrasound.26,45 However, ultrasound is less expensive and involves no ionizing radiation. It is a suitable alternative for monitoring the progress of lesions during therapy.

 |
 |
|
Figure 7a: MRI-demonstrated transformation of hepatosplenic candidiasis lesions. Axial T2-weighted fat suppressed image reveals multiple small high-intensity microabscesses (arrows) scattered throughout liver and spleen.
Reprinted with permission, Semelka, et al. Am J Roentgenol 1997;169:1311-6.
|
Figure 7b: Transverse sonogram of the liver in a patient with hepatosplenic candidiasis showing a wheel-within-a-wheel microabscess at the portal vein (arrow).
Reprinted with permission, Samuels, et al.45
|
Figure 7b: Unenhanced abdominal CT scan showing low attenuation microabscesses in both liver and spleen.
Reprinted with permission, Nucci personal communication.
|
Course Number: V035D
This CME Expires on July 1, 2005; no tests will be accepted after this date.
This course is accredited by
The University of Pittsburgh School of Medicine, Center for Continuing Education and The International Immunocompromised Host Society
|
 |

