The possibility of fungal infection, as well as bacterial infections, in hospitalized patients must now be considered by clinicians. Candida now surpasses Enterobacter, Pseudomonas, and E coli and is the fourth leading cause [8] of BSI sepsis (Fig 2). The clinician’s ability to identify high-risk factors for fungal infection will guide decisions regarding prophylaxis, diagnosis, and treatment.
It is important to realize that there is no such thing as a standard risk of fungal infection; patients must be assessed individually. The degree of risk and the factors most likely to predispose the patient to fungal infection differ between patient populations and are largely determined by interaction between exposure to the infecting organism and the net state of immunosuppression. The balance between the immune and nonimmune defenses is often of pivotal importance. Profoundly immunocompromised but infection-free individuals can rapidly develop devastating fungal disease if mucocutaneous barriers are disrupted.
Many events or factors can help identify patients at high risk of developing a fungal infection before, during, or after a period of hospitalization. The type of immunocompromiseaffecting, or likely to affect, the patient as a consequence of treatment can enable the clinician to predict which mycoses are likely to occur [18]. Neutropenic patients are at high risk of developing invasive mycoses. However, it is important to realize that neutropenia per se is not a good predictor of infection risk; the magnitude and duration of the neutropenia are the determining factors (Fig 6).
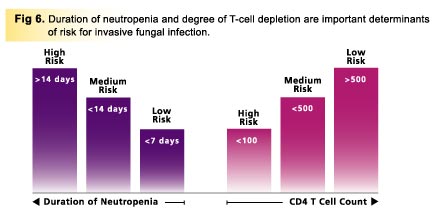 Chemotherapy-induced neutropenia of short duration (<7 days) should not require antifungal prophylaxis during treatment cycles. However, patients in whom intensive chemotherapy leads to prolonged neutropenia have a high incidence of invasive fungal infection. Duration of neutropenia is shorter in autologous bone-marrow recipients than in allogeneic recipients, and this is reflected in a lower incidence of fungal infection in the autologous group [34]. CD4 lymphocyte depletion due either to AIDS or to immunosuppressive therapy increases the risk of infection, and the degree and time scale of this depletion provide valuable guidelines for antifungal therapy and prophylaxis (Fig 6).
Chemotherapy-induced neutropenia of short duration (<7 days) should not require antifungal prophylaxis during treatment cycles. However, patients in whom intensive chemotherapy leads to prolonged neutropenia have a high incidence of invasive fungal infection. Duration of neutropenia is shorter in autologous bone-marrow recipients than in allogeneic recipients, and this is reflected in a lower incidence of fungal infection in the autologous group [34]. CD4 lymphocyte depletion due either to AIDS or to immunosuppressive therapy increases the risk of infection, and the degree and time scale of this depletion provide valuable guidelines for antifungal therapy and prophylaxis (Fig 6).
Underlying medical conditions and diseases including hyperglycemia, uremia, and malnutrition are important considerations, since they can cause or amplify defects in host defenses.
Course Number: V035B.043001
This CME Expires on July 1, 2003; no tests will be accepted after this date.
This course is accredited by
The University of Pittsburgh School of Medicine, Center for Continuing Education
|

